Sinoatrial and Atrioventricular Conduction Defects
Sinoatrial (SA) conduction abnormalities could be first degree, second degree or third degree SA blocks. But it is not possible to identify first degree and third degree SA blocks on the surface ECG as the sinus node activity is not visible. Theoretically first degree SA block would mean prolongation of SA interval with regular conduction and third degree SA block would mean total absence of SA conduction.
Second degree SA block
Second degree SA block could by either type I or type II. In type I SA block there will be progressive prolongation of SA interval followed by blockage of one P wave. This will manifest as progressive shortening of PP interval followed by a pause. But the pause will not be exact double of regular PP interval.
In type II SA block, there will be sudden blockage of a P wave so that a sinus pause exactly twice the regular PP interval will be noted.
Sinus arrest or pause
Sinus arrest is a sinus pause which is more than one and half times the regular PP interval, but not exactly twice the PP interval. There is no preceding progressive shortening of PP interval. Sinus arrest/pause is not a SA conduction, abnormality, but a defect in the automaticity of the sinus node.
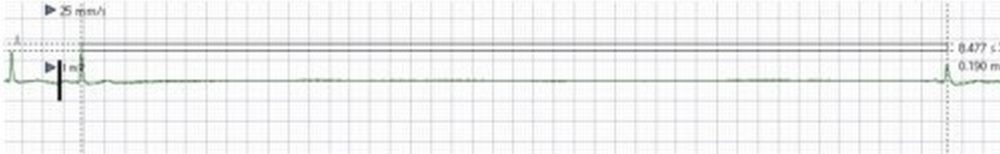
ECG rhythm strip documenting a long sinus pause of around 8.5 seconds. Such long pauses would indicate suppression of sinus node activity and is a manifestation of sick sinus syndrome. Pauses more than 3 seconds while awake, would indicate implantation of a permanent pacemaker, provided reversible causes can be ruled out. Occasionally long pauses can occur during sleep, which need not have the same significance as pauses which occur while awake. Pauses during sleep can be recognized only by continuous monitoring by either Holter or event recorders. Long pauses can occur during termination of a tachyarrhythmia, classically after termination of atrial fibrillation in a tachy-brady syndrome. This is because of down regulation of pacemaker current (If current, also known as funny current) by the prolonged tachycardia. This is why pauses on termination of tachycardias do not have the same weightage as spontaneous pauses regarding indication for permanent pacemaker implantation. Some such pauses may not recur after ablation of the tachycardia focus.
PR interval gets progressively prolonged, suggesting second degree type I AV block. But the pause is not containing a P wave because of associated second degree SA block. The pause helps the AV junction to recover and the next cycle starts with a normal PR interval. Such combination of dual nodal disease is seen in structural nodal disease as well as in the acute phase of inferior wall myocardial infarction.
Modern day intensive care monitors have facility to record ECG rhythm data for a few days, depending on the software and memory capacity. Hence it is possible to retrieve the cardiac rhythm data after an event for documentation and analysis. This facility is usually restricted to bedside monitors which are connected to a central console. Standalone bedside monitors seldom have long term storage facility. We can review data from the central monitor console depending on the events automatically logged by the device as well as scroll through the timeline to see events at a particular time. Print outs and electronic storage of the tracings are possible.
Central monitor record capturing a long pause of about 8 seconds and two pauses of around 2 seconds. The underlying rhythm is atrial fibrillation and there is some QRS widening with a notch. Overall this suits a diagnosis of tachy-brady syndrome and warrants a permanent pacemaker, provided a reversible cause can be excluded. Capturing such a record obviates the need for Holter monitoring in this case. Long term anticoagulation has to be considered if the CHADS2 score is high.
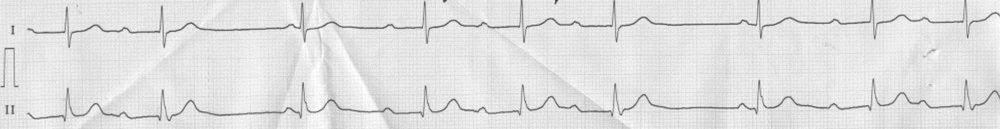
Sinus bradycardia with first degree AV block. RR interval of 1280 ms, corresponding to a heart rate of 47 per min and PR interval is 320 ms.
First degree AV block
First degree atrioventricular block (AV block) is manifested in the ECG as prolongation of the PR interval. Normal PR interval ranges from 120 – 200 ms. First degree AV block is a very common finding and if isolated, does not carry additional prognostic significance. But if it is associated with other conduction abnormalities like bundle branch blocks, it gives added significance, indicating a more severe conduction system disease.
Second degree AV block
Second degree AV block can be either Mobitz type I or type II. Type I is also known as Wenckebach phenomenon. Mobitz type II block is usually associated with intraventricular conduction defects like right bundle branch block, bundle block, hemiblocks or a combination of these.
Mobitz type I (Wenckebach phenomenon)
Typical features of Wenckebach phenomenon are:
- Progressive prolongation of PR interval followed by a dropped QRS.
- Progressive shortening of RR intervals.
- This is because the increments in PR interval are decremental.
- Pause due to dropped QRS is less than twice the previous RR interval.
Mobitz type I block is usually more benign and due to AV nodal pathology. Progression to complete AV block is less common. Even if it progresses to complete heart block, the escape rhythm is of narrow QRS and has a good rate. Second degree AV block associated with inferior wall infarction is Mobitz type I. Conduction ratio in second degree AV block is mentioned as the ratio between the number of P waves in a Wenckebach cycle and the number of QRS complexes. For example, if 3 P waves are conducted and the 4th one is blocked, it is called as 4:3 Wenckebach block. In Wenckebach type of block, the conduction ratio is always in the form of x+1:x, that is only one P wave is non conducted in any cycle. Highest grade of type I AV block possible is 2:1 AV block, in which the ventricular rate will be half that of the atrial rate.
Mobitz type II
In Mobitz type II second degree AV block, there is no progressive prolongation of PR interval. Instead there is an abrupt droppage of a QRS. Hence the pause is exactly twice the previous RR interval and there is no variation in RR intervals except for the pause. There may be no prolongation of baseline PR interval. Mobitz type II block usually originates below the His bundle and as mentioned earlier, is associated with other intraventricular conduction defects. It carries a more sinister prognosis as the escape rhythm which occurs if it progresses to complete heart block is of wide QRS, lower rate and unstable.
Mobitz type I (Wenckebach phenomenon)Mobitz Type I Second degree AV block – 3:2 Wenckebach: There is a limitation in interpreting the rhythm as a long rhythm strip is not available. This is often the situation when the ECG is obtained without your direct supervision. The PR interval of the first beat is quite prolonged so that it overlaps with the T wave of the previous beat. The next P wave is superimposed on the T wave as well as non-conducted, resulting in a pause. The PR interval of the second beat is less prolonged as the conduction recovers partially following the blocked beat and the pause. The next PR interval is again prolonged. So overall the ECG shows a 3:2 type I AV block. QRS complex is narrow, indicating a supra Hisian location of the block. These features fit in with the Wenckebach phenomenon.
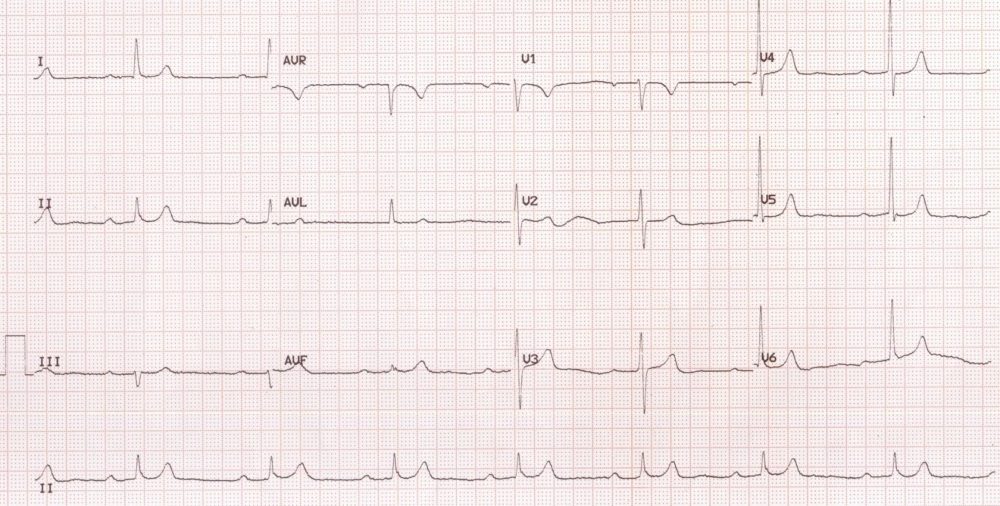
Advanced AV block with RBBBAdvanced AV block with RBBB: PP interval is 480 ms, corresponding to an atrial rate of 125/min. PR interval is relatively fixed, at 440 ms for most of conducted beats, though the conduction ratio varies between 3:1 and 2:1 (two P waves visible between 2nd & 3rd and 5th & 6th QRS complexes in the rhythm strip. QRS complex is wide with rsr’s’ pattern in V1 and slurred S waves in lateral leads indicating right bundle branch block. Q waves and T inversions are noted in inferior leads. In the setting of inferior wall infarction, though supra Hisian type of block (type I) is more likely, RBBB would indicate a type II AV block. Electrophysiology study is needed in this case to delineate the exact physiology.
Advanced AV block
When two or more consecutive P waves are non-conducted, it is termed advanced AV block. Advanced AV block is midway between usual second degree AV block and complete AV block.
Complete AV block
In complete AV block, there is no relation between the atrial and ventricular rhythms and they are completely dissociated. The four classical ECG criteria for diagnosis of complete AV block are:
- Regular PP interval.
- Regular RR interval.
- PP interval shorter than RR interval (atrial rate more than ventricular rate).
- Totally varying PR interval (indicating AV dissociation).
Though the PP intervals and RR intervals are usually regular, there could be some variations occasionally. If there is an occasional conducted beat the ventricular rhythm can show irregularity. Junctional focus can have slight variation in rate due to autonomic influence. Atrial rates can show two types of sinus arrhythmia. In respiratory sinus arrhythmia, PP interval shortens during inspiration as the rate increases and lengthens during expiration as the rate decreases. In ventriculophasic sinus arrhythmia, a PP interval enclosing a QRS complex will be shorter. This is thought to be due to the mechanical effect of ventricular systole causing enhanced pulsation of the sinus node artery penetrating the sinus node [1]. It has been shown that the ventriculophasic response can be enhanced by deep inspiration like in the case of sinus arrhythmia [2].
The location of block in complete AV block can be either above (supra Hisian) or below the bundle of His (infra Hisian). In supra Hisian block, the QRS complex is narrow and has a relatively higher rate as it arises from the lower part of the AV junction. In infra Hisian block, the subsidiary focus is from the ventricle and has a lower rate with wide QRS complex. The subsidiary rhythm in supra Hisian AV block is more stable than that in infra Hisian block. Hence there is a higher chance for Stokes Adam attacks with infra Hisian block. In the setting of acute myocardial infarction, supra Hisian block is usually noted with inferior wall infarction and infra Hisian block is associated with anterior wall infarction. The latter is often associated with significant left ventricular dysfunction and poorer prognosis because of the large area of myocardial damage involved. Supra Hisian complete heart block in inferior wall infarction is usually reversible. Infra Hisian complete heart block in the setting of anterior wall infarction is more likely to be permanent. Even if there is partial recovery, very often bundle branch or fascicular blocks remain.
References
- Dadu RT, McPherson CA. The ventriculophasic response: relationship to sinus arrhythmia and the duration of interposed QRS complexes. Ann Noninvasive Electrocardiol. 2013 Jul;18(4):336-43.
- de Marchena E, Colvin-Adams M, Esnard J, Ridha M, Castellanos A, Myerburg RJ. Ventriculophasic sinus arrhythmia in the orthotopic transplanted heart: mechanism of disease revisited. Int J Cardiol. 2003 Sep;91(1):71-4.
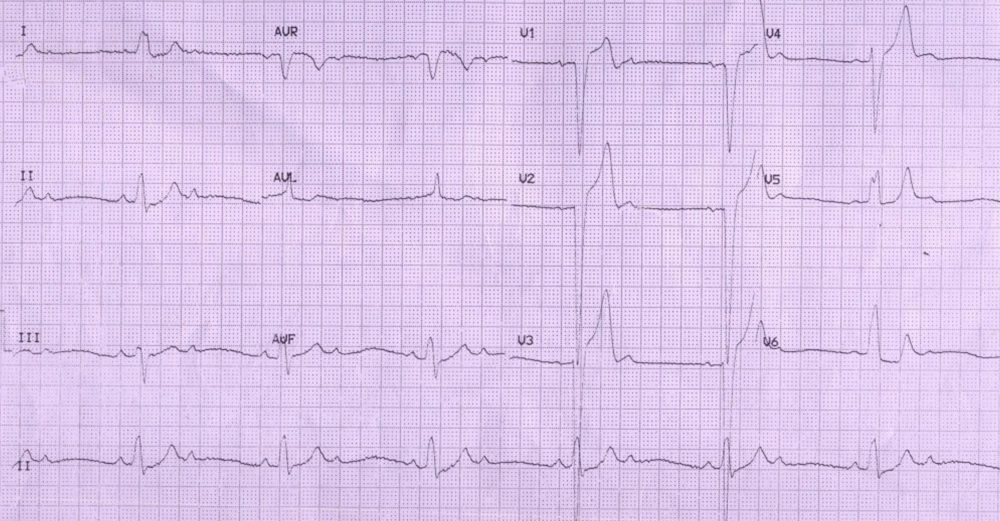
ECG tracing showing severe bradycardia due to complete heart block. RR interval is 1.8 s, corresponding to a ventricular rate of 33 per minute. PP interval is 720 ms, indicating an atrial rate of 83 per minute. The T waves are very broad and the QT interval is prolonged (760 ms), suggesting the potential for torsades de pointes and Stokes Adam attacks.
There are two P waves for every QRS complex, with atrial rate double that of ventricular rate, denoting 2:1 AV conduction (2:1 AV block). In addition there are features of left bundle branch block.
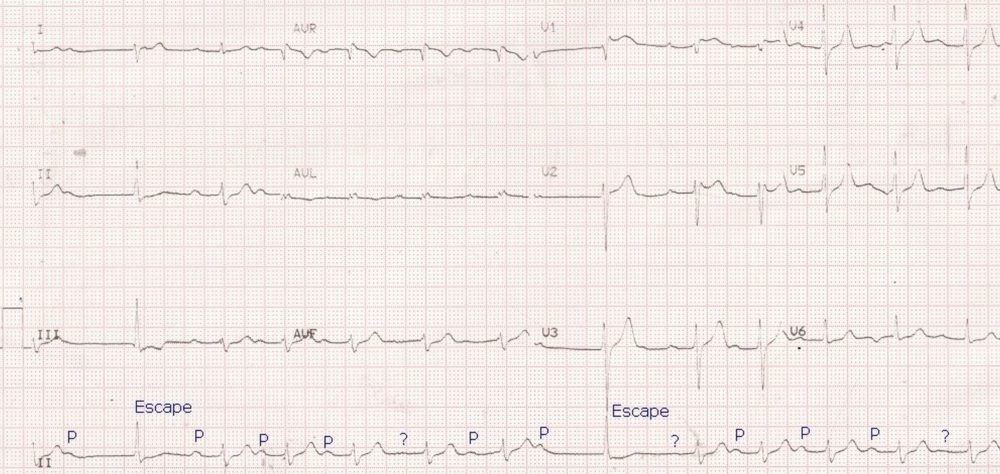
Intermittent AV block with escape beats: Basic PR interval is prolonged to about 320 ms. Some P waves marked as “?” in the lead II rhythm strip are fairly well seen in the other simultaneously recorded leads, with morphology similar to the regular P waves. Some P waves appear to be non conducted, producing a pause which is terminated by a different type QRS complex. These QRS complexes have been marked as escape beats, possibly junctional beats with aberrant conduction as they are not wide enough to be called ventricular escape beats. The escape beats occur at almost the expected time of the next P wave. It may be that the P waves are masked by the simultaneously occurring QRS complexes. The escape beats do not reset the basic sinus cycle, which continues as before. Though the P wave after the second escape beat is not visible in lead II rhythm strip, it is well seen other simultaneously recorded leads. Change in P wave morphology in lead II may also suggest a shifting in the pacemaker focus in some beats, which can only be identified by multi electrode intracardiac recording. This is because the P wave amplitudes in surface leads are small so that minor changes in morphology between beats may not be easily appreciated.
Response to exercise in congenital complete heart block
Usually response to exercise is poor in acquired complete heart block. This is because most often the subsidiary focus in adult onset complete heart block is ventricular, which has an intrinsically slower rate poor response to exercise. But in congenital complete heart block, the block is usually supra Hisian and the subsidiary focus is junctional and has a higher escape rate. It also responds fairly well to exercise. The following sequence of ECGs demonstrates this well.
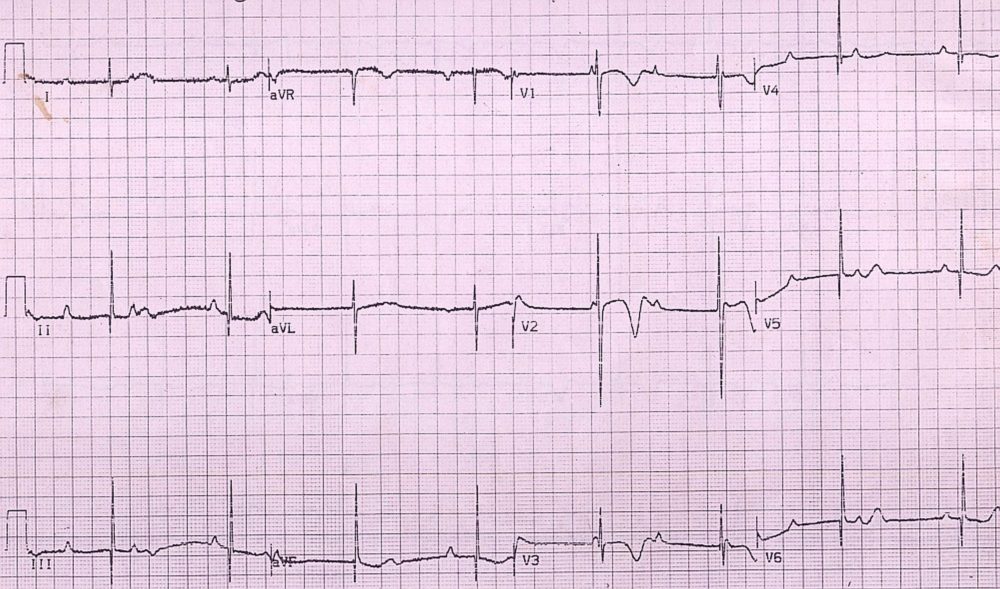
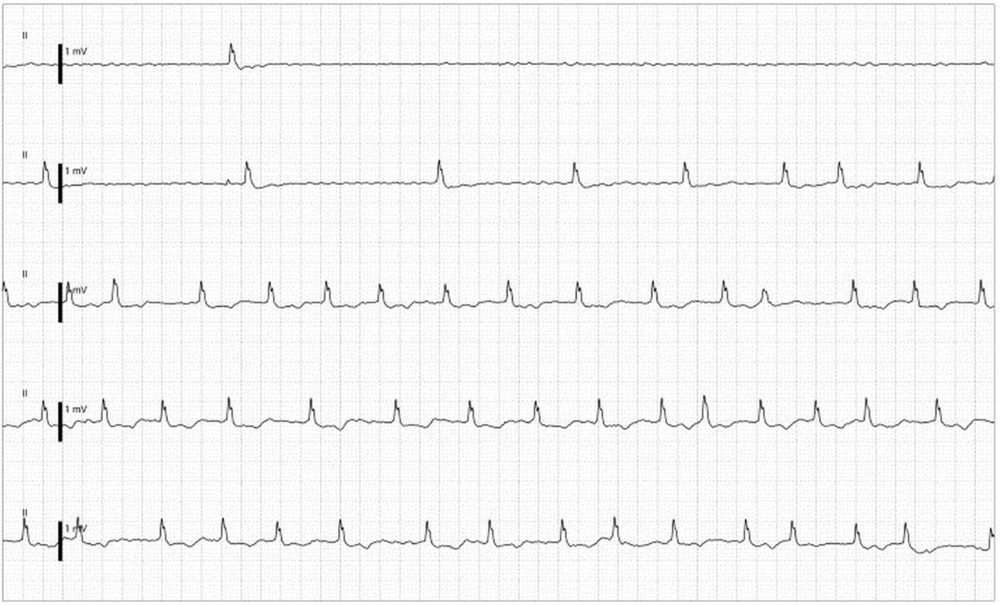
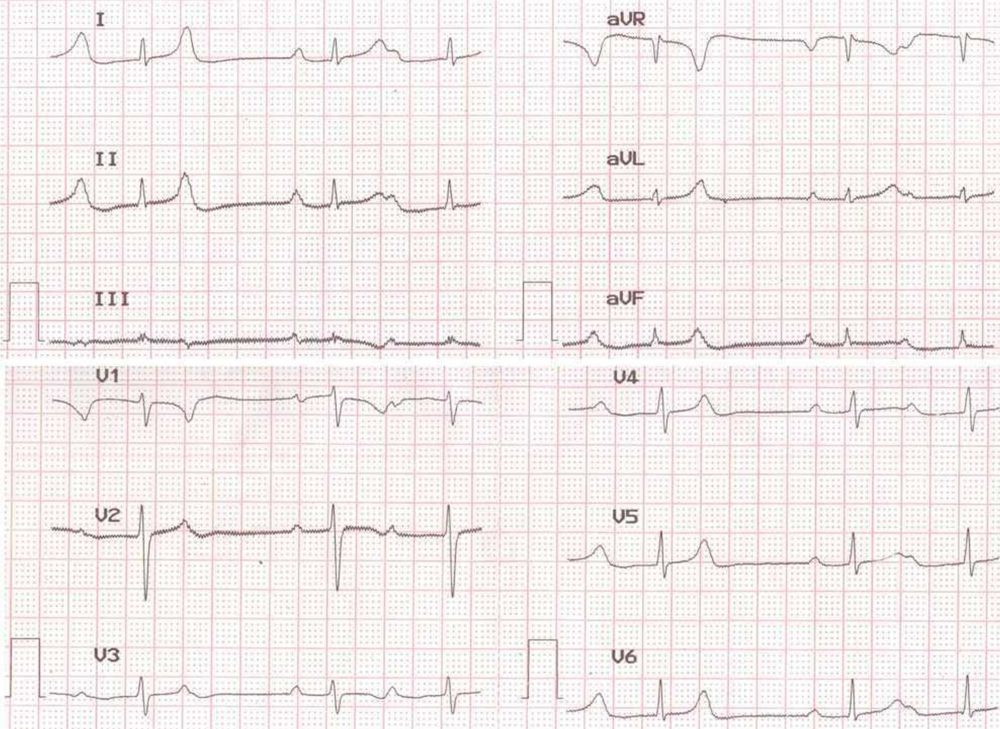
Congenital complete heart block with RR interval of 1280 ms (ventricular rate: 47/min) and PP interval of 960 ms (atrial rate of 62.5/min). The four criteria four diagnosis of complete heart block are satisfied: regular PP interval, regular RR interval, PP interval less than RR interval and varying PR interval. QRS is narrow, indicating supra Hisian location of the complete heart block, with a junctional focus capturing the ventricle. Such a situation in a young boy indicates congenital complete heart block. An exercise test is useful in assessing the response of the heart rate to exercise (below).
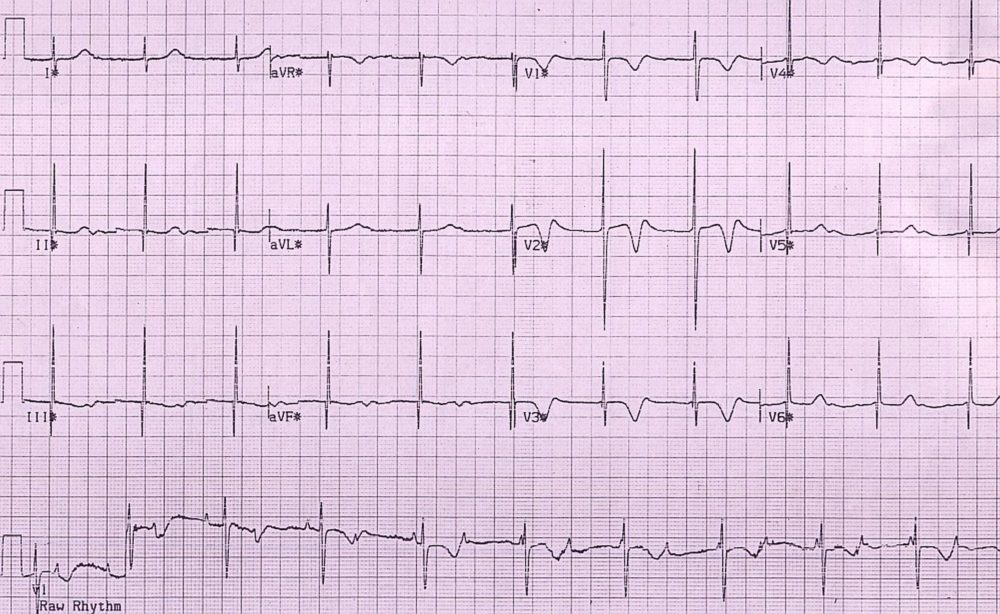
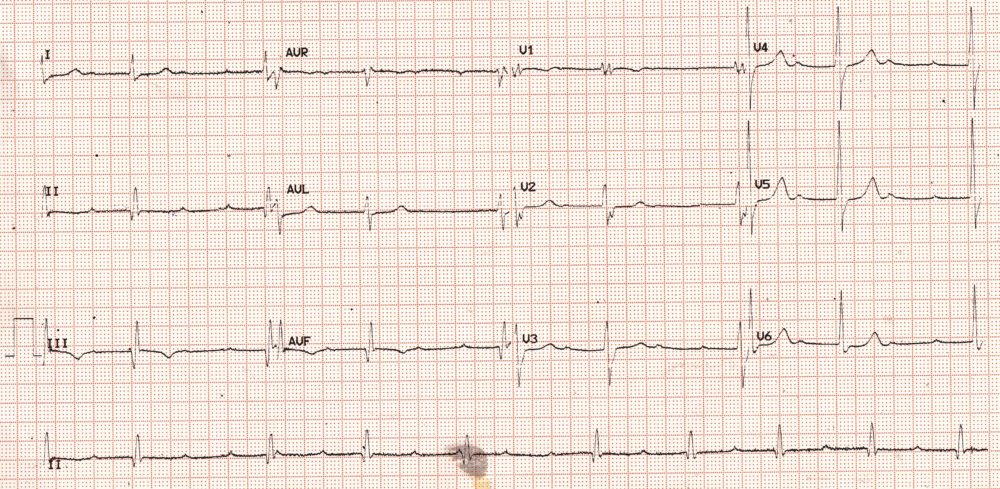
In stage 1 of exercise, the PP interval has shortened to 600 ms (atrial rate: 100/min) and RR interval is 1000 ms (ventricular rate: 60/min). There is progressive change in atrial and ventricular rates with exercise, though the response is blunted compared to sinus rhythm with regular conduction. (Please observe the raw rhythm strip at the bottom of the tracing). The peak exercise recording is given below.
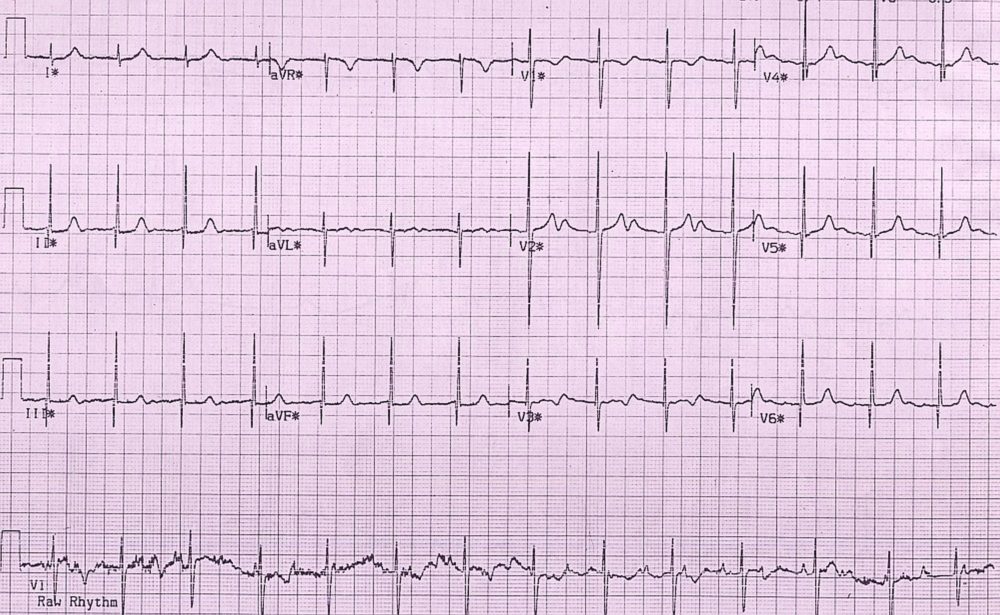
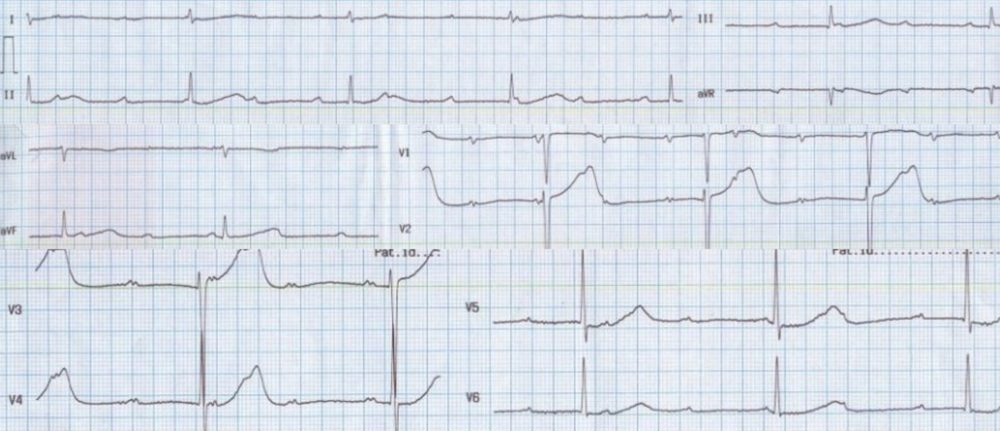
Peak exercise tracing in congenital complete heart block with PP interval 400 ms (atrial rate: 150/min) and RR interval of 720 ms (ventricular rate: 83/min). (Please observe the raw rhythm strip at the bottom of the tracing).